How hormone repalcement therapy affects your skin while you’re transitioning
We spoke to dermatologists for the technical side of things, and members of the trans community for some more personal insight. Members of the trans community, specifically those on hormone replacement therapy (HRT), can face a number of skin-related challenges throughout their transitions. For instance, taking testosterone may lead to severe breakouts, while taking estrogen can potentially clear the skin. But as Emily, who uses they/them pronouns and prefers to go by their first name in this story for privacy reasons, told HuffPost, there’s more to it than just physical changes. “Dealing with skin issues might seem like an insignificant thing or like something everyone has to deal with, but I think when you’re trans you often have to spend a huge amount of mental energy concerned with how other people are perceiving your physical form,” they said. “For me, being able to feel like I have some control over the face I present to the world makes a big difference in terms of my confidence and overall mental health.” Skin care, and more specifically, how to take care of your skin and what to expect from your skin throughout the transition process, is something that’s not widely talked about. To learn about what happens to the skin during a transition, we spoke to dermatologists for the technical side of things, and three members of the trans community, including Emily, for some more personal insight.
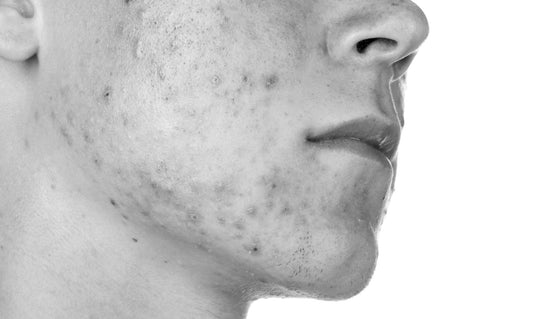
Here’s what you should know about taking testosterone: Dr. Brian Ginsberg, a board-certified dermatologist based in New York City, told HuffPost that most of the skin changes trans people experience are a result of the hormones each individual is taking. Those taking testosterone to masculinize their appearance typically see an increase in body hair and facial hair along with a decrease in scalp hair, Ginsberg said. With that increase in facial hair, an individual taking testosterone may also end up with ingrown hairs and folliculitis, Dr. Jennifer MacGregor, of Union Square Laser Dermatology in New York, added. “These are all easy to treat in the office with laser (if desired), topical medications and short courses of oral antibiotics for severe cases,” MacGregor said via email. “The most severe acne may also respond to isotretinoin (Accutane) to prevent scarring.” As Ginsberg pointed out, however, those who want to take isotretinoin to treat severe acne may run into a few difficult hurdles. The regulations surrounding use of the medication require individuals to register with an FDA-regulated program called iPledge, for which people need to register according to their biological sex as opposed to their gender identity. Many trans male patients (understandably) refuse to register as female, “especially after the journey they may have gone through to come to define themselves as male,” Ginsberg added. For the most part, taking isotretinoin while on testosterone is considered safe, Ginsberg said. However, another potential hurdle is the fact that some surgeons require patients to be off the medication for a certain amount of months before a surgical procedure ― including both top and bottom surgery ― which could affect one’s plans. “Patients should be aware of this when taking isotretinoin and planning for future procedures, and should speak with their surgeons prior to starting isotretinoin,” Ginsberg said.
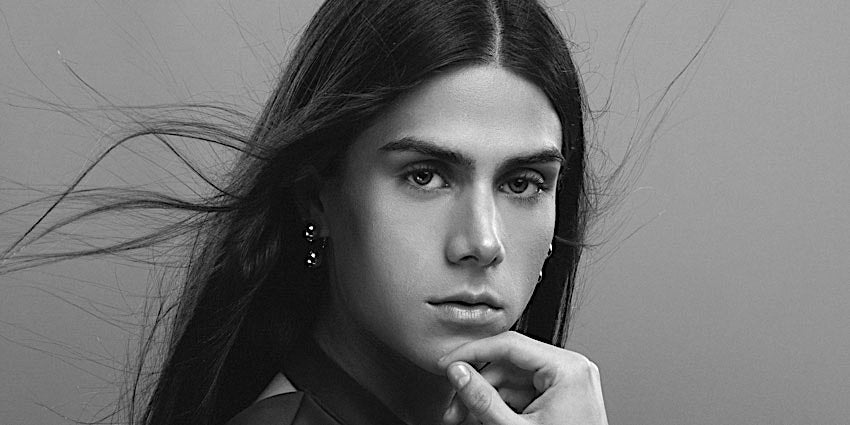
Here’s what can happen if you’re taking estrogen: While acne and increased body and facial hair are common for those taking testosterone, MacGregor and Ginsberg said that individuals taking estrogen may experience the opposite. In some cases, that might mean an individual sees their skin clear up. Ginsberg said that estrogen can potentially help with breakouts, specifically if your acne is related to your body’s oil production; taking estrogen can decrease oil production. Male to female transition can also result in thinning facial hair, MacGregor said, noting that laser hair removal is often desired by patients who want smooth skin. It’s important to note that while the hair may get thinner, it won’t completely go away, according to Ginsberg. Issues like scarring, dry skin and rashes may also occur, MacGregor said, noting those should be treated by a well-trained dermatologist.
Take it from individuals who’ve gone through it: In order to get a real sense of what it’s actually like to experience the skin issues that may come along with transitioning, we sought insight from three individuals who’ve been there.
Oliver: “I think probably within the first three to six months of taking testosterone, I noticed my skin changed the most,” said Oliver Whitney, a former HuffPost employee who’s been taking testosterone for a year and a half. Whitney, who uses they/them pronouns, said the most noticeable change was that they were getting acne breakouts. “It was kind of different than the breakouts I would get in high school, which is probably the last time I had acne in a way that was noticeable and annoying,” they said, adding that their skin also became oilier on testosterone. When it came to treating their acne, Whitney said they didn’t really know what to do, “because I didn’t have a really good skincare regimen.” However, they did say they’d been aware of the potential of HRT-related breakouts from speaking to other trans people and reading blogs. Still, they said, the whole experience “was kind of like being in high school again and having breakouts and feeling really insecure and awful about it, as you feel when you’re a teenager.” Whitney also had to get used to shaving their facial hair while also dealing with acne, something they found challenging. Figuring out what products to buy to treat acne while you’re also having to shave “is a whole other world,” they said.
Emily, who has been taking testosterone for a little over 14 months, also experienced an increase in breakouts as a result of HRT. They explained that while they had some mild acne as an adult, HRT led to large and painful cystic breakouts “that were unlike anything [they’d] experienced before testosterone.I also developed new acne patterns on my face (chin and forehead, which were not problem areas previously) as well as next-level body acne, especially on my back and shoulders,” Emily said via email. “At around a year on testosterone my acne started to get better, but I don’t know if that was a natural adjustment to the hormones or due to my skin care regimen.” Emily also said they’ve “always been obsessed with skin care” and has tried different products for both acne and for anti-aging and hydration. They also use a prescription antibiotic face cream, which they said was difficult to get from their primary care physician or nurse practitioner; the providers wanted them to see a dermatologist first, but Emily said that would have required a referral and long wait for an appointment. “As a trans person, I already spend a lot of time as it is going to doctors appointments (and paying copays!),” they said via email, adding, “When I eventually got [the prescription] I’m pretty sure it made a huge difference on my acne.”
AJ Clementine, a Melbourne, Australia-based YouTuber who who’s been on HRT for three years ― taking Progynova (estradiol, a form of estrogen) and spironolactone ― told HuffPost the change in hormones helped her skin. “I was pretty lucky with my genetic lottery, she said, adding that she “didn’t suffer from crazy amounts of breakouts throughout puberty” and experienced only a few breakouts before she started transitioning at age 19. “Since I started HRT I never really get any breakouts and if I do it’s a pimple every four months,” she said. For Clementine, getting clear skin was a perk she didn’t really expect to happen during her transition period, and she’s well aware that her situation might not be universal. “Every transition is different and just because I happened to get clear skin doesn’t mean every trans woman will get clear skin on HRT,” she said.
The right skin care regimen is different for everyone: “One thing I’ve learned from all of my patients is never to assume what they want, what they see in the mirror or what their goals might be,” MacGregor said, noting that gender doesn’t define one’s preference for their appearance. “Everyone has their own unique anatomy, attributes, gifts, strengths and weaknesses. Everyone has their own unique ideas about inner and outer beauty and their own goals for how to achieve their best self,” she added. “As physicians and providers we can listen to our patients, create a friendly and safe space so they can teach us, then strive to provide the best possible outcome.” All three individuals who shared their experiences said they had never gone to a dermatologist to address HRT-related skin issues. Whitney explained that while they’d like to see a dermatologist, they’d be hesitant if that provider didn’t have experience treating the skin issues trans people face on HRT. Meanwhile, Emily expressed some frustration about seeking dermatological help, as it often required a doctor referral and and led to long wait times just for appointments. Both MacGregor and Ginsberg agreed that the relationship between dermatologists, and perhaps medical professionals in general, and the trans community hasn’t always been the most welcoming. “I think, unfortunately, many individuals in the community have had poor experiences with providers in the past, whether that’s the provider not fully understanding the process, the provider using the wrong pronouns or something worse,” Ginsberg said. “A lot of this unfortunately is something that stays with you and is a big hurdle going into it.” He recommended seeking out trans-friendly care, whether through word of mouth or organizations like Gay and Lesbian Medical Association (GLMA) and MyTransHealth that provide lists of suitable providers nearby. From his experience, he said, providers are open to treating members of the trans community, “but are frankly uninformed.” MacGregor agreed, “Not all clinicians have extensive training and depending on state laws, some practitioners have little to no training or experience.” As these topics become more widely discussed, we can only hope that both medical providers and members of the trans community (and LGBTQ community as a whole) can get access to the information they need to prepare them for all the parts of their transition. As Emily put it, “I hope all trans people feel like they deserve to define what looking and feeling their best means for them.” (By Julia Brucculieri from HuffPost.com)
WHAT TO
READ NEXT
STAY IN
TOUCH
Sign Up and be among the first to learn about new mìsula announcements and products.
- Choosing a selection results in a full page refresh.
- Opens in a new window.