What causes ITP (Idiopathic Thrombocytopenic Purpura)?
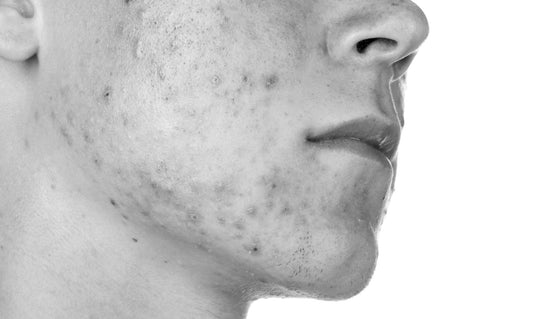
If you’ve ever discovered a mysterious bruise on your body, you’ve probably tried to retrace your steps. Maybe you slammed into that doorknob harder than you thought, or maybe stumbling to the bathroom in the dark for a midnight pee break was a bad idea. But if you have the bleeding disorder immune thrombocytopenia (also known as idiopathic thrombocytopenic purpura or just ITP), you might find yourself wondering where the hell this new bruise came from way too often. Bruising is a common sign of ITP, as are symptoms like petechiae (small dots of blood that look like a skin rash), sudden bloody noses, gums that bleed out of nowhere, and more, according to the National Heart, Lung, and Blood Institute (NHLBI). But what causes someone to get this disorder in the first place? Let’s take a look at what experts know about ITP causes—and what they don’t. ITP happens when your immune system accidentally targets platelets. As you might already know, your immune system is your body’s basic line of defense against disease. When your body perceives a threat, like the influenza virus your coworker just sprayed into the air via a forceful sneeze, your body ideally produces an immune response to neutralize it. Hats off to the human body for this super useful mechanism. But, unfortunately, your immune system isn’t infallible, meaning it can accidentally interpret something that’s not harmful—or something that’s even helpful—as a threat, which experts believe is what happens with ITP. If you have ITP, it means your immune system targets platelets, which are cells in your body that cause blood to stick together (or clot), the NHLBI explains. If someone doesn’t have ITP and gets a cut, their body directs platelets to the wound to form a clot that helps stop the bleeding. Clearly, if your body is attacking such a useful component of your blood, things can get a little tricky. For some context, the average platelet count for adults is between 150,000 to 450,000 per cubic millimeter of blood. If someone’s platelet count falls below 100,000 per cubic millimeter of blood and doctors cannot pinpoint an external cause like medications, they can be diagnosed with ITP. That doesn’t necessarily mean they’d experience symptoms, though. That appears to be more of an issue for people with platelet levels that fall below 50,000. ITP is a relatively rare blood disorder, with estimates in the American Journal of Hematology suggesting that 3.3 per 100,000 adults receive an ITP diagnosis annually and that anywhere from 1.9 to 6.4 per 100,000 children are diagnosed each year. A bacterial or viral infection can trigger ITP. Before we dive into that, quick note: ITP can be acute, meaning symptoms last for six months or fewer, or it can be chronic, which is when symptoms last more than six months, according to the NHLBI. Many ITP cases, especially those that occur in children, are acute ones that happen after a viral infection like the mumps or the flu, the Mayo Clinic says. This is because as the body is trying to fight off the infection, it might also start destroying platelets, Elizabeth Roman M.D., a pediatric hematologist and oncologist at New York University Langone Health, tells SELF. It’s not just kids: Adult patients sometimes mention that they had some kind of infection before getting diagnosed with ITP, Rahki Naik, M.D., M.H.S., associate director of hematology and oncology fellowship program at Johns Hopkins Medicine, tells SELF. Infections like HIV and hepatitis can trigger the illness, as can H. pylori (a bacteria that causes stomach ulcers), the Mayo Clinic says. However, when adults are diagnosed with ITP, the onset is often spontaneous and the condition tends to be chronic, Dr. Naik explains. Other autoimmune disorders can be a factor as well. We already know that ITP can be either acute or chronic, but it can also be broken down into two other categories. With primary ITP, no other disorders or causes are present. Secondary ITP, on the other hand, means the disorder occurs alongside other autoimmune disorders like lupus, which is a condition where the body attacks tissue and organs, Sjorgen’s Syndrome, which occurs when the body attacks the glands that make tears and saliva, and seemingly in rarer cases, rheumatoid arthritis, which is when the body attacks its own tissues including joints. In a 2016 retrospective study published in Medicine, researchers looked at 85 ITP patients in a rheumatology department and found that 33 of those patients had lupus, 16 of them had Sjogren's Syndrome, and three had rheumatoid arthritis. It isn’t clear why autoimmune disorders happen alongside ITP, but it’s not super surprising since ITP basically comes about when your immune system goes rogue. Anyone who’s been pregnant knows that there’s pretty much no end to how many ways your body can change throughout the process. As it turns out, ITP can become more intense than usual during pregnancy, according to the Merck Manual. It’s unclear exactly what causes this reaction primarily because pregnant people tend to experience other conditions that might result in platelet loss, including gestational thrombocytopenia, which is when a pregnant person’s blood platelet count falls for no apparent reason, and preeclampsia, which is a blood pressure condition that can also contribute to lower platelet levels. Treating ITP depends on the cause. ITP has a surprisingly great prognosis for many people: Most children recover spontaneously within six months of diagnosis, and many adults with chronic ITP find that their symptoms normalize spontaneously within five years, according to the Merck Manual. So, if you have mild ITP, your doctor might not recommend any treatment and simply wait to see if your body decides to boost your platelet count over time. But if you have a more severe form of ITP, your doctor might recommend treatment. There isn’t a cure for ITP, which can be frustrating, but there are various medications out there to increase platelet counts or calm your immune system, according to the Mayo Clinic. If your body isn’t responsive to medication, your doctor might recommend a splenectomy, which is a surgery to remove your spleen (which is mainly what creates the antibodies that attack platelets), the NHLBI explains. If you have a bacterial or viral infection, the NHLBI says that doctors might attempt to treat that in the hopes that your platelet count will rise. Similarly, in cases where secondary ITP is present, treatment varies depending on the underlying illness. When it comes to pregnancy and ITP, doctors are most concerned with managing the increased risk of heavy bleeding during delivery, according to the Mayo Clinic. Your doctor may decide to give you a medication to temporarily increase your platelet levels before childbirth, the Merck Manual explains. No matter exactly what’s causing your ITP, it’s generally a manageable illness. Talking to your doctor can help you maintain your quality of life—and cut back on those annoying random bruises as much as possible. (Source: Self.com)
WHAT TO
READ NEXT
STAY IN
TOUCH
Sign Up and be among the first to learn about new mìsula announcements and products.
- Choosing a selection results in a full page refresh.
- Opens in a new window.